Benign Brain Tumors
An acoustic neuroma (vestibular schwannoma) is generally a slow growing, benign tumor that arise from the eighth cranial nerve (nerve that deals with balance and hearing). Patients with these tumors often report trouble with balance, vertigo, tinnitus (ringing in ear) and progressive loss of hearing. When tumors are small (2 cm or less), patients may consider options of waiting to observe growth pattern with serial scans, surgery to remove the tumor, or Gamma Knife radiosurgery to treat the tumor. Factors that influence what treatment to select include: patient’s age and general medical condition, size of tumor, degree of hearing loss, neurologic symptoms.
While many patients with small tumors decide to avoid any treatments, it is important to consider that 70% of patients have measurable growth over 5 years and 95% at 10 years. Most commonly, tumor growth is estimated about 1-3 mm/year in at least one plane. Even though modern MR scans are quite impressive, measuring growth in one plane only may overlook the importance of considering the entire volume of the tumor. Precise determination of growth over time requires detailed, high-resolution MR scans.
Recent studies have documented that the “observe” option may have higher rates of hearing loss over time than those who select Gamma Knife treatment at time of diagnosis. Patients who underwent treatments had useful hearing rates of 77%, 7-%, and 64% at 3,4, and 5 years; those who chose to wait and observe had useful hearing preservation rates of 75%,52% and 41% at 3, 4, and 5 years.
Reports of efficacy of Gamma Knife radiosurgery for acoustic neuromas show a 98% long term tumor control rate (10 years). Over time, 73% of patients show some decrease in size of tumor, while 25% of patients showed no change in tumor size. 2% of patients had surgery because follow up scans showed increase in tumor size. Best hearing preservation is found in patients with small tumors.
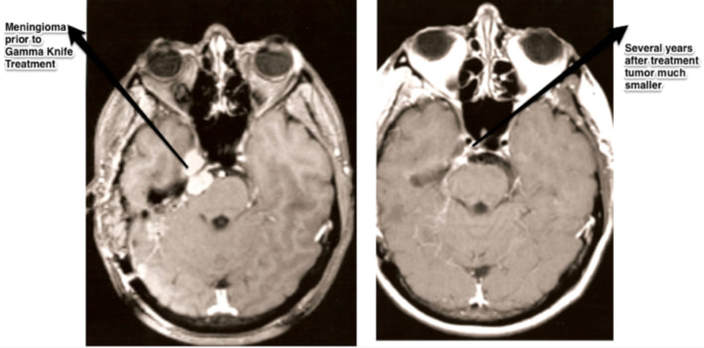
Gamma knife radiosurgery in the modern era show very low rates of complications of facial numbness or facial paralysis after treatment (< 5%). Meningiomas are benign tumors that arise from the coverings around the brain. Meningiomas are more common in women. For many patients, surgery to remove the lesion is preferred. However, meningiomas may be situated in areas of the brain that make removal hazardous or even impossible. Radiosurgery may be helpful in selected patients. Radiosurgery is not recommended for large tumors or tumors on the optic (vision) nerve when there is intact vision. The Gamma Knife allows precise targeting to the tumor with blocking of radiation to optic chiasm or other vital areas as appropriate. The goal of Gamma Knife treatment for meningiomas is to control future growth. Over 10 years after treatment, 44% of tumors show decrease in size while 52% show no change. In a few patients (about 4%), tumors may enlarge in spite of Gamma Knife treatment. Gamma Knife treatment for meningiomas may be used as the only (primary) treatment or as adjuvant therapy after previous surgery. If scans after surgery show residual tumor, Gamma Knife treatment is recommended over observation for most patients.
Metastic Brain Tumor
Metastatic tumors to the brain constitute the single most common indication for Gamma Knife use around the world. The goals of treatment include: preservation or improvement of brain function, preservation of life, reduced use of steroids, and reduction of side effects. The decision to treat metastatic disease to the brain involves several considerations: tumors are often circumscribed; survival relates often to how well disease is controlled in other parts of the body. Selected large tumors may be treated with surgery.
Gamma knife radiosurgery allows the ability to treat multiple areas of metastatic disease and In the past decade, increasing clinical evidence and guidelines support the use of radiosurgery. In any one patient, a full discussion with knowledgeable radiation oncologist and neurosurgeon is necessary to decide about use of Gamma Knife radiosurgery, open surgery, or even whole brain radiation. The team at Los Robles Neuroscience Gamma Knife center has many years of experience in helping inform patients about the goals and risks of all these important decisions.
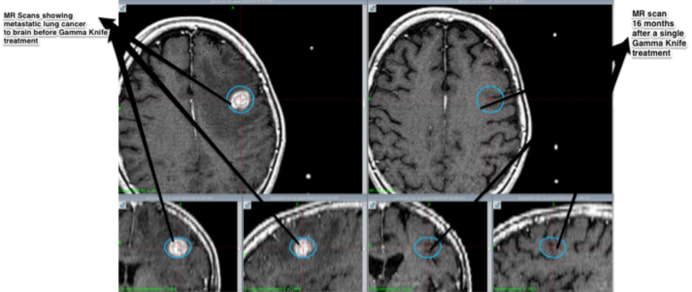
MR Scans showing metastatic tumor to the brain (lung cancer) before and 16 months after a single Gamma Knife therapy session.
Whether or not to use whole brain radiation as substitute or in addition to Gamma Knife radiosurgery is an important question that requires a conversation among patient, radiation oncologist and neurosurgeon. As a general policy, we believe that Gamma Knife treatment is a preferred first line option, will control 80-90% of tumors treated, preserves cognitive function, and can be repeated as needed for future metastatic tumors. Multiple metastatic tumors can also be treated.